
From a patient perspective, breast reconstruction is one of the most rewarding plastic surgical procedures available today. New medical techniques and devices help your plastic surgeon to create breasts that are more natural than at any previous time in history. Reconstructed breasts can actually feel warm, soft and supple. The scarring has also been minimized to reduce the stigmata of breast surgery.
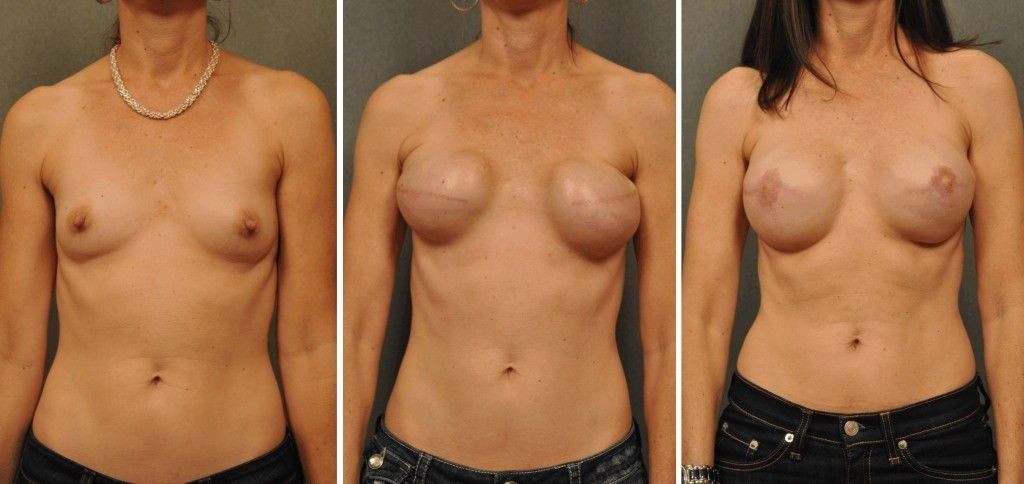
Whereas in the past, breast reconstruction was delayed for months to years after the mastectomy, reconstructions are now usually performed at the same time as breast removal (mastectomy). This allows the patient to wake up with her new breast already in place. This has proven to be a huge boost to our patients’ sense of wholeness and self-image; our patients are spared the experience of seeing themselves with no breast at all.
Determining Your Candidacy for Breast Reconstruction
The majority of patients are considered good candidates for immediate breast reconstruction. However, there are some who are advised to delay reconstruction: patients with serious medical problems such as heart disease; patients with very large, aggressive breast tumors, or patients who cannot decide if they want breast reconstruction. Most general surgeons will refer you to a plastic surgeon prior to surgery, to determine whether you are a good candidate for immediate breast reconstruction.
Skin Sparing Mastectomy
The essential components of a mastectomy include the removal of all of the breast glandular tissue, and the nipple and areola. Depending on the type of breast tumor you have, lymph node removal or sentinel lymph node biopsy may be necessary. In the old days, general surgeons removed all of the skin of the breast. This skin removal was a throwback to the days before breast reconstruction when general surgeons removed all breast skin so that no sagging skin would be left on the chest following mastectomy. In approximately 1996, the concept of skin-sparing mastectomy was introduced into medical practice. Dr. Lee is proud to have been among the first surgeons in the San Diego area to adopt this new concept. Since breast cancer is a disease of the breast glandular tissue and is not a disease of the skin, one can safely and completely perform a mastectomy by removing the nipple/areola complex and glandular tissue and leaving all the skin of the breast in place. By leaving all of the breast skin in place, Dr. Lee is able to perform much more realistic breast reconstructions without the extensive scarring associated with older type mastectomies. You should discuss with your general surgeon ahead of time whether or not you are a candidate for a skin-sparing mastectomy.
Breast Reconstructive Procedure Descriptions
Breast reconstructions can be divided into three main groups: breasts reconstructed using implants, breasts reconstructed with your own body tissues (flap reconstructions), and breasts reconstructed with a combination of your own tissue and an implant. There are different benefits and risks associated with each of the above options. A detailed consultation with Dr. Lee will help you to determine which option is best suited to you and your lifestyle.
Breast Reconstructions
This common technique combines skin expansion and the subsequent insertion of a breast implant. Following a mastectomy, your surgeon will insert a partially filled implant tissue expander beneath your skin and chest muscle. The implant is placed partially deflated to prevent excessive tension on the skin edges during the healing process. After you have healed, he/she will begin the expansion of the implant. This “expansion” procedure is done in the office by injecting saltwater (saline) through a tiny needle into a small valve mechanism buried beneath the skin. Expansions are started about 10 to 14 days after the placement of the expander implant. Two or three expansions are usually required, spaced one to two weeks apart. After the skin over the breast area has stretched enough, the expander may be removed in a second operation and a more permanent implant will be inserted. Some expanders are designed to be left in place as the final implant. The nipple and the dark skin surrounding it, called the areola, are reconstructed in a subsequent procedure.
If radiation therapy is planned for you following mastectomy, an implant reconstruction is probably not the most appropriate choice for you. Radiation therapy can cause hardening or contracture in up to half of the patients treated. Make sure you inform your surgeon if radiation therapy is a planned part of your treatment.
Flap Reconstruction
One of the greatest advances in breast reconstruction is the movement of one’s own vascularized tissue from one part of the body to another (flap reconstruction). Such tissue commonly comes from locations where patients have excess tissue such as the abdomen, back, or buttocks.
The tissue transferred to create the breast must maintain its blood circulation in order to maintain its viability. This is accomplished in one of two ways. The flap tissue can be left attached to its original blood supply (pedicle flap) and tunneled beneath the skin to the chest, where it can be sculpted into a breast mound. Alternatively, the tissue can be completely cut “free” from the abdomen or buttocks (free flap) and then transplanted to the chest by reconnecting the blood vessels to new ones in that region using a microvascular technique. This latter option must be performed by plastic surgeons adept in microsurgery. Dr. Lee has over 20 years of experience performing hundreds of similar procedures.
Breasts reconstructed entirely with your own tissue are generally more natural in appearance and texture since both the native breast and the transferred tissue are comprised mostly of fat. The transferred tissue can be sculpted to closely match the other side” an advantage not available with implant reconstructions. If the abdominal tissue is used, you will have the added benefit of an improved abdominal contour from the tummy tuck done to remove the abdominal tissue. Regardless of whether the tissue is tunneled beneath the skin on a pedicle or transplanted to the chest as a microvascular free flap, this type of surgery is more complex than skin expansion, and recovery will take longer than with an implant.
Dr. Lee is aware of all of these procedures and will recommend the best procedure for you.
TRAM Pedicle Flap
Transverse Rectus Abdominis Myocutaneous Pedicle Flap
This flap is one of the most popular tissue reconstructions performed today. Its name is derived from the place on the abdomen where it comes from. Skin, fat, and muscle from the lower abdomen are raised. A tunnel is created under the upper abdominal skin to the breast cavity. The TRAM flap is then passed through the tunnel to the breast cavity where it is sculpted into a breast. The flap is left attached to its blood supply during this transfer (pedicle flap), and a tummy tuck is performed at the abdominal donor site.
TRAM Free Flap
Transverse Rectus Abdominis Myocutaneous Free Flap
This procedure must be done by a plastic surgeon with extensive experience in microsurgery. Its name is derived from the place on the abdomen where it comes from. Skin, fat, and muscle from the lower abdomen are completely removed from the body. This tissue is then sculpted side by side with the mastectomy specimen to create a realistic breast. The tissue is then inserted into the breast cavity and is connected to the chest blood supply to re-establish its circulation using a microsurgical technique. A tummy tuck is performed at the abdominal donor site. The advantages of this operation over the pedicle TRAM flap are a two to three-fold higher blood flow to the flap (assuring better flap healing), less muscle harvested from the abdomen, and no visible bulge in the upper abdomen (since the tissue is not tunneled under the abdominal skin). The disadvantages over a pedicle TRAM flap are that this flap is more technically demanding, requires close post-operative monitoring, and risks flap loss if the circulation in the flap should stop (1.5% risk).
DIEP Free Flap
Deep Inferior Epigastric Perforator Free Flap
This flap is the newest addition to free flap breast reconstruction. It is basically very similar to the TRAM Free Flap procedure. The main difference is that during the harvesting of the flap from the abdomen, the entire rectus abdominis muscle is spared and left in place in the abdomen. Thus, the transferred tissue consists only of skin, fat, and the blood vessels that supply the tissue. This tissue is then sculpted side by side with the mastectomy specimen to create a realistic breast. The tissue is then inserted into the breast cavity and is connected to the chest blood supply to re-establish its circulation using the surgical technique. This is a very technically challenging procedure and should only be performed by a plastic surgeon expert in microsurgery. A tummy tuck is performed at the abdominal donor site. The advantage of this operation over the pedicle TRAM flap is that no muscle is harvested from the abdomen, and no visible bulge appears in the upper abdomen (since the tissue is not tunneled under the abdominal skin). The disadvantages over a pedicle TRAM flap are that this flap is more technically demanding, requires close post-operative monitoring, and risks flap loss if the circulation in the flap should stop (2% risk).
Gluteal Free Flap
In this procedure, your Changes surgeon will harvest buttock tissue along with its delicate blood supply from the patient, and then sculpt it side by side with the mastectomy specimen to give a very nice shape to the new breast. The new tissue is then inserted into the breast cavity and is reconnected to the chest blood supply using a microsurgical technique. The donor site is closed leaving an oblique scar on the buttocks. This free flap is very difficult and is considered as a backup procedure when other techniques are unsuitable for the patient.
Latissimus Dorsi Pedicle Flap
Originally described in the 1970s, this flap has stood the test of time. It serves as a very safe, predictable, and reliable source of tissue for breast reconstruction. The skin, fat, and latissimus dorsi muscle are raised off of the back. A tunnel is created from the back, through the armpit, to the breast cavity. The latissimus dorsi flap is then passed through the tunnel into the breast pocket where it is sculpted into a new breast. The flap is left attached to its blood supply during transfer, making it a pedicle flap. Because of limited muscle size, the flap is often too small to recreate a breast symmetric with the opposite side. Therefore, an implant is often placed underneath the flap to make it larger. The main downside to the latissimus dorsi flap is the need to harvest a muscle from the back, a visible scar which is left on the back, and the need for an implant.
Combination Reconstructions
Most breast reconstructions can be accomplished by using either implants or one’s own tissue alone. However, when the medical situation mandates the use of one’s own tissue, and that tissue is inadequate in size to build asymmetric sized breast, then an implant (silicone or saline) may be placed under the flap tissue to help gain adequate size. Dr. Lee will be able to tell you during your consultation if you have adequate tissue for breast reconstruction.
Follow-Up Procedures
Most breast reconstruction involves a series of procedures that occur over time. Usually, the initial reconstructive operation is the most complex. Follow-up surgery may be required to replace a tissue expander with an implant or to refine the shape of the reconstructed breast and to reconstruct the nipple and the areola. Quite often we recommend an additional operation to enlarge, reduce, or lift the opposite breast to match the reconstructed breast. In California, surgery on the opposite breast, which is necessary to gain symmetry with the reconstructed breast, is covered by your insurance plan. Most follow-up procedures are performed on an outpatient basis
Pre-Operative Planning
You can begin talking about reconstruction as soon as you’re diagnosed with cancer. Dr. Lee will always work with your breast surgeon to develop a strategy that will put you in the best possible condition for reconstruction.
After evaluating your health, your Changes surgeon will explain which reconstructive options are most appropriate for your age, health, anatomy, tissues, goals, and lifestyle. Be sure to discuss your expectations frankly with your surgeon. He will be equally frank with you, describing your options and the risks and limitations of each. Post-mastectomy reconstruction can improve your appearance and renew your self-confidence, but keep in mind that the desired result is a movement, not perfection.
You will be advised on the anesthesia plans, the facility where the surgery will be performed, and the costs. Health insurance policies vary regarding the amount of coverage for post-mastectomy reconstruction. Check your policy to make sure you’re covered and to see if there are any limitations on what types of reconstruction are covered.
Along with your oncologist, Dr. Lee will give you specific instructions on how to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain vitamins and medications. While making preparations, be sure to arrange for someone to drive you home after your surgery and to help you out for a few days, if needed.
Recovery
It may take you up to six weeks to recover from a combined mastectomy and flap reconstruction. If implants are used alone, your recovery time may be less.
Reconstruction cannot restore normal sensation to your breast, but in time, some feeling may return. Most scars will fade substantially over time, though it may take as long as one to two years. The better the quality of your overall reconstruction, the less distracting you’ll find those scars.
Follow your surgeon’s advice on when to begin stretching exercises and normal activities. As a general rule, you’ll want to refrain from any overhead lifting, strenuous sports, and sexual activity for three to six weeks following reconstruction.
Chances are, your reconstructed breast may feel firmer and look rounder or flatter than your natural breast. It may not have the same contour as your breast before mastectomy, nor will it exactly match your opposite breast. But these differences will be apparent only to you. For most mastectomy patients, breast reconstruction dramatically improves their appearance and quality of life following surgery.
Read More Breast Reconstruction Articles
Not all breasts look the same, we are sure you know that by now. Take a look at our blog on five totally normal breast shapes!
Part of breast reconstruction is nipple reduction. Learn more about the nipple reduction surgery and if you should include it within your breast reconstruction procedure in San Diego.